SEOUL, August 04 (AJP) - KAIST researchers have discovered how inflammation in the placenta during pregnancy can alter a baby's immune system, leading to stronger allergic reactions such as asthma after birth. The study is the first in the world to show exactly how this prenatal inflammation affects immune development and raises new possibilities for early prediction and prevention of childhood allergic diseases.
The findings were announced on August 4 by KAIST, whose research team was led by Professor Lee Heung-kyu from the Department of Biological Sciences. According to the team, inflammation in the mother's body during pregnancy can influence the fetus through the placenta by disrupting its ability to regulate stress hormones. This, in turn, changes how the baby's immune system develops, especially the activity of T cells, a type of white blood cell that plays a central role in the body's immune memory.
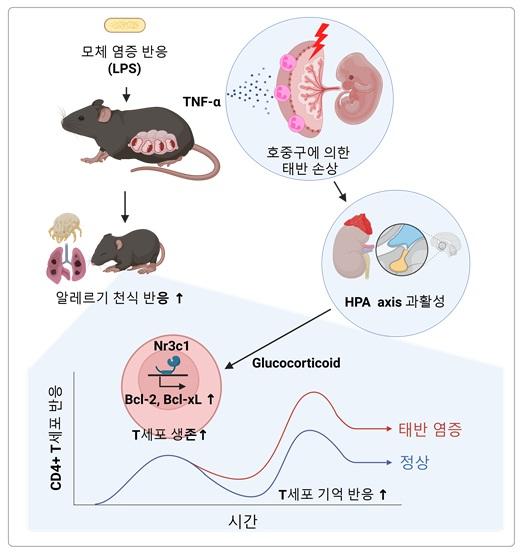
The researchers conducted an experiment using pregnant mice. To create an inflammatory condition, they injected the animals with a toxin called lipopolysaccharide (LPS), which is commonly used to trigger immune responses in lab studies. As expected, the inflammation spread to the placenta.
The team found that the inflamed placenta produced increased levels of tumor necrosis factor alpha (TNF-α), a chemical signal that activates neutrophils. Neutrophils are immune cells that form the largest portion of white blood cells in the human body, making up between 40 to 75 percent. They play a key role in the body's innate immune system by attacking bacteria and fungi. When neutrophils became active in the placenta, they caused tissue damage, which triggered stress in the fetus.
As a result, the fetus began producing large amounts of a stress hormone known as glucocorticoid. This hormone caused a shift in the development of the fetus's immune system. Specifically, the T cells in the fetus, immune cells responsible for remembering threats like viruses or allergens, lived longer and developed stronger memory functions.
After birth, this change had consequences. When these offspring were repeatedly exposed to allergens such as house dust mites, their immune systems reacted more aggressively than usual. The mice showed strong eosinophilic inflammation, a type of allergic response that plays a key role in asthma. Eosinophils are immune cells that become overactive in people with allergies and contribute to inflammation and tissue damage.
"Through this study, we were able to demonstrate for the first time how a mother's immune response during pregnancy, particularly inflammation, affects the allergy-related immune system of the fetus through the placenta," said Lee Heung-kyu. "This will serve as a scientific basis for developing early detection biomarkers and preventive strategies for childhood allergic diseases."
The first author of the paper is Kwon Myung-seung, a Ph.D. graduate of KAIST's Graduate School of Medical Science and Engineering and currently a clinical fellow in gynecologic oncology at Konyang University Hospital. The study was published on July 1 in the journal Mucosal Immunology, a leading publication in the field of immune responses related to the body's mucous membranes.
The paper is titled Placental inflammation-driven T cell memory formation promotes allergic responses in offspring via endogenous glucocorticoids. The research was supported by the Ministry of Science and ICT and the National Research Foundation of South Korea, under the Basic Research Program and the Biomedical Technology Development Program.
Copyright ⓒ Aju Press All rights reserved.